If constant bloating, gas, diarrhoea or constipation are things you find yourself struggling with on a regular basis, it might be time to start thinking about your gut bacteria.
Small Intestinal Bacterial Overgrowth (SIBO) is an increasingly recognised condition that disrupts digestion, nutrient absorption, and affects overall gut health. Despite its impact, many individuals often go undiagnosed or are mistakenly treated for other gut-related conditions instead.
But SIBO doesn’t just stop at digestive discomfort. It can also trigger a range of unexpected issues, from brain fog and headaches to increased allergies, sudden lactose intolerance, stomach noises, and unexplained weight changes. Recognising these lesser-known symptoms - and tracking when they appear - can be a crucial step toward understanding what’s really going on in your gut.
But first - what actually is SIBO?
SIBO occurs when bacterial colonies typically found in the colon (large intestine) colonise the small intestine. Because the small intestine isn’t designed to control those microorganisms, the overgrowth disrupts normal digestion, prevents nutrient absorption and gut motility and leads to a range of unpleasant symptoms.
There are three types of SIBO, categorised based on the dominant gas produced by the overgrowth of bacteria.
- Methane-dominant (IMO - Intestinal Methanogen Overgrowth) → Linked to constipation, bloating, slow digestion and weight gain.
- Hydrogen-dominant → Typically causes diarrhoea, bloating and low nutrient status due to malabsorption. This can then link to fatigue and weight loss.
- Hydrogen sulphide-dominant → Often associated with foul-smelling gas, diarrhoea, brain fog and an increase in food sensitivities.
How can I tell which SIBO might be causing the problems?
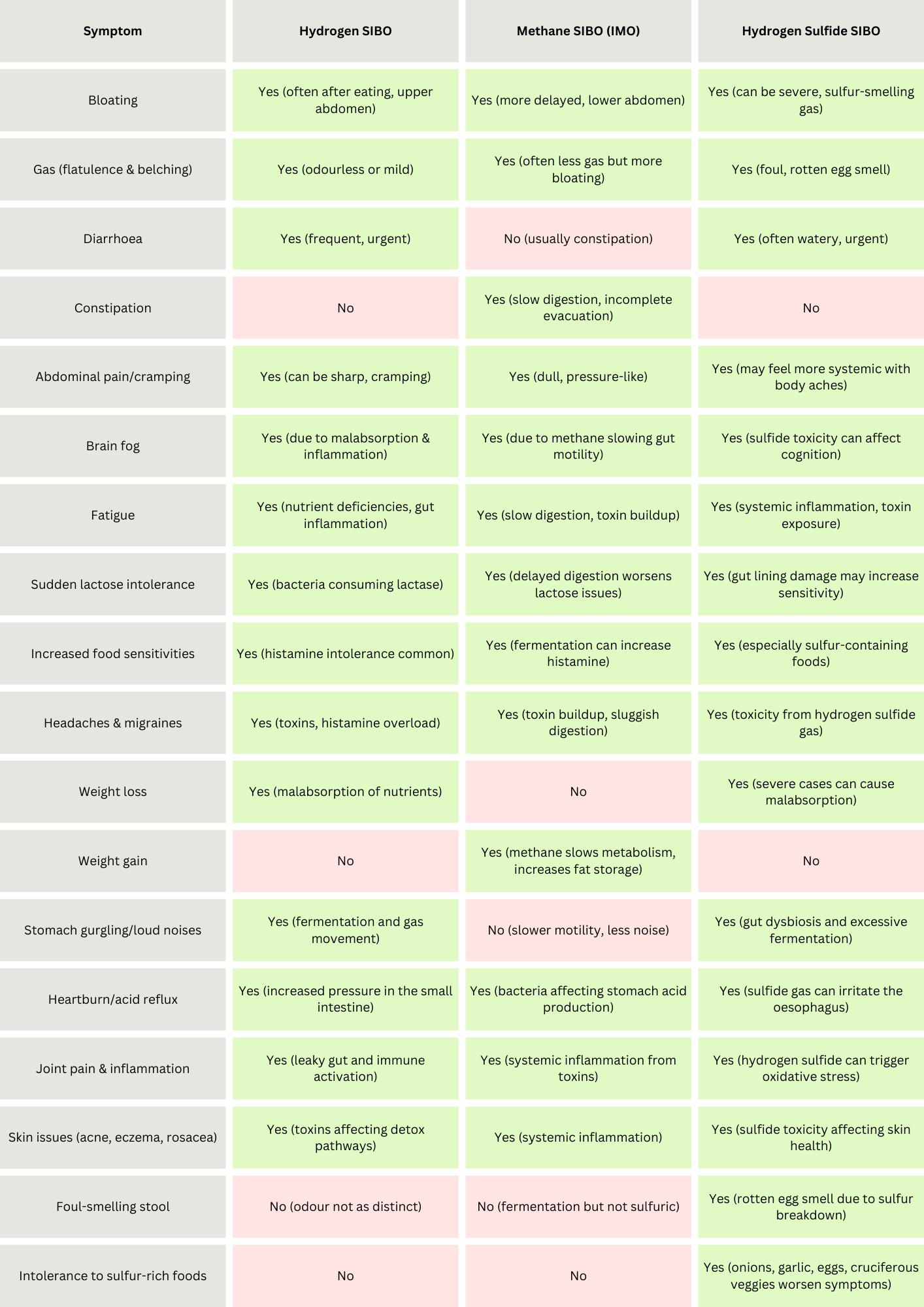
SIBO isn’t a one-size-fits-all condition. Each type of SIBO affects digestion and overall health in different ways, and can present in a variety of symptoms - which is where my handy symptom table comes in. Below you can find a breakdown of the key symptoms associated with each type, helping you identify which one might be contributing to your gut issues.
How do I know it’s not something else?
Good question! SIBO is often mistaken for other things - like chronic acid reflux, Irritable Bowel Syndrome (IBS), fungal overgrowth, or histamine intolerance. In this case it’s best to focus on symptom management as the treatment strategy.
The most common examples of missed or mis-diagnosis are:
- Irritable Bowel Syndrome (IBS). Research suggests between 60-80% of IBS cases are actually caused by SIBO.
- IBS-D sufferers → 70-80% have SIBO (usually hydrogen or hydrogen sulphide SIBO).
- IBS-C sufferers→ 30-60% have SIBO (often methane-dominant SIBO).
- IBS-M (Mixed type): Varies, but around 50-70% have SIBO.
- Candida/fungal overgrowth. Both SIBO and Candida can cause bloating, body pain, headaches and brain fog, but there are some key differences to differentiate between the two. See the table below for a more detailed comparison, but some key Candida symptoms to look out for are: bloating after eating sugar-rich foods, sugar cravings, and oral or genital thrush. If you’re suffering from gas, fatigue, bloating after fermentable fibre, or have food sensitivities, it could be SIBO.
- H. pylori infection. This bacterial infection affects stomach acidity and causes chronic heartburn/reflux, bloating and excessive fullness after meals, burping, nausea, and slower gut motility leading to intermittent bowel movements. A key difference is timing. Issues with the stomach from H. pylori will present pretty immediately on eating, whereas there is a slight delay with SIBO. However, if someone has very active SIBO, the force of upward pressure from excess gas in the small intestine immediately after food could also create the above symptoms. H. pylori can also be linked to chronic sinusitis, lots of mucus production, hoarseness and chronic coughs which SIBO wouldn’t usually cause
- Food intolerances. SIBO can lead to reactions to FODMAPs, dairy, sulphurous and histamine-containing foods, making it easy to misdiagnose. Food intolerances as an immune response occur due to changes in the lining of the intestines and are more inflammatory or stress related in origin. Comparatively, SIBO causes issues with the function of the gut and excess fermentation, and can be triggered more intensively by certain foods. Both, however, can cause inflammatory skin issues and increased allergy symptoms.
Is full recovery possible?
The good news is that absolutely yes, you can treat it. However relapse rates are high if treatment is not addressed through a multi-faceted approach. It’s not just about eliminating the overgrowth bacteria, but also reconditioning the small intestinal environment to prevent recurrence in future. We also need to understand why you might have ended up with SIBO in the first place.
Classic antibiotic therapy, as prescribed by a gastroenterologist, has an incredibly low efficacy rate, and can often create extremely unpleasant side effects without actually resolving the original symptoms. This is because antibiotics don’t provide the necessary support for gut motility or toxin removal - so as the bacterial overgrowth dies, its toxins continue to circulate around the body, causing flu-like symptoms, body aches, migraines, nausea and intense fatigue.
Instead, I use a five step process to understand the root cause, treat the symptoms, and prevent relapse.
- Assessment. Usually a glucose and lactulose breath test are used to determine the type of SIBO. As I have been working in chronic and complex digestive health for 10+ years, in some cases I will forgo this if I can clearly see someone has SIBO. This saves the need to use the sugar-rich solution usually used for the breath test, which actually increases the activity of bacteria and can cause symptoms to worsen.
- Dietary Adjustments. I take a person-centred approach to diet, and design a bespoke plan for each client, depending on symptom-relief and lifestyle. Usually this means starting off with a low fermentable fibre diet, removing dairy and fruit for the short-term, and focusing on simple meals centred around whole food ingredients.
- Gut Motility Support. Before adding in any kind of antimicrobial, good and stable gut motility must be established. For diarrhoea-dominant SIBO, those stools need to be slowed and formed; for constipation-dominant SIBO, stools need to get moving to allow for proper toxin excretion.
- Antimicrobials to target the overgrowth. The type of antimicrobials depend upon the type of SIBO, and they are always used with a progressive opening of someone's diet, to concurrently restore normal function and prevent recurrence.
- Addressing Root Causes. This happens all the way through - the story of how someone got there is the key to the puzzle! Often root causes turn out to be things like chronic stress, colonic irrigation, or chronic constipation due to poor dietary habits. Unravelling these causes, and the habits around foods that occur as a result, is actually what frees someone from the SIBO cycle.
When should I seek help?
As soon as you feel something isn’t right! Many people endure digestive symptoms for years, assuming they’re just an unavoidable part of life. But in as little as 6–8 months, I’ve helped individuals become completely symptom-free. Conditions like IBS are often dismissed as ‘common’, leading people to adapt their lives around discomfort, for example always needing to know where the nearest toilet is or avoiding food for hours before going out to prevent bloating.
You should seek advice if:
- Digestive symptoms persist for more than a few weeks despite dietary changes.
- Bloating, gas, or irregular bowel movements significantly affect your daily life.
- You experience unexplained weight loss, nutrient deficiencies, or worsening food intolerances.
How can I prevent SIBO in the first place?
- Eat at a regular intervals and leave good gaps between meals to allow your digestive system to regulate itself. Avoid grazing/snacking!
- Make your meals textural so you chew thoroughly. Be aware when you’re eating, and try to incorporate bitter foods at the start of your meals like nuts, seeds and bitter leaves like rocket.
- Manage stress and invest in your sleep quality. If our body is under-rested or stressed then our digestive system becomes less effective and more vulnerable. We also see lower levels of good gut bacteria which will make us more susceptible to opportunistic overgrowth and issues with bowel motility.
- Address underlying digestive conditions including GERD, low stomach acid and past infections as these will increase vulnerability.
- Eat a diverse diet rich in whole foods and minimal - if any - ultra processed foods, as this ensures your natural microbiome will be diverse, numerous and protective.
If any of the symptoms we’ve covered in this post sound familiar to you, please don’t wait to reach out. Book a confidential quick consult with me here for an immediate discussion, or opt for the Liebling Health Digestion Package (call or email based), for personalised nutritional and lifestyle guidance over four sessions, in addition to any targeted supplements.
.png)
.png)

.png)
.png)


.png)





